Fracture Nomenclature for Pisiform Fractures
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Pisiform Fracture, the historical and specifically named fractures include:
Pisiform dislocation and fracture-dislocation
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the carpal bones account for ~6% of fractures overall and up to 18% of all hand fractures. The vast majority (58-89%) occurs in the scaphoid, while fractures of the other 7 carpals are uncommon, comprising ~1.1% of all fractures. The pisiform is a small, pea-shaped bone located in the most ulnar position of the proximal carpal row, and its superficial position makes it vulnerable to direct trauma, but the incidence of pisiform fractures is only 0.2-2% of all carpal fractures. Half of pisiform fractures occurs in isolation; the other half is concomitant with other wrist injuries, such as a perilunate dislocation, distal radius fracture, or additional carpal fracture. These injuries may result from a direct blow, tendon avulsion, or microtrauma, and the exact mechanism may be difficult to determine. However, falls on an outstretched hand (FOOSHs) and sporting accidents are frequently responsible. As with other carpal injuries, pisiform fractures can be difficult to recognize on routine radiographs, and the diagnosis may therefore be missed upon initial examination. Conservative treatment using early immobilization is indicated for nondisplaced pisiform fractures, while surgery is typically needed for displaced fractures and cases that fail conservative treatment, with pisiform excision being the preferred surgical intervention.1-5
Definitions
- A pisiform fracture is a disruption of the mechanical integrityof the pisiform.
- A pisiform fracture produces a discontinuity in the pisiform contours that can be complete or incomplete.
- A pisiform fracture is caused by a direct force that exceeds the breaking point of the bone.
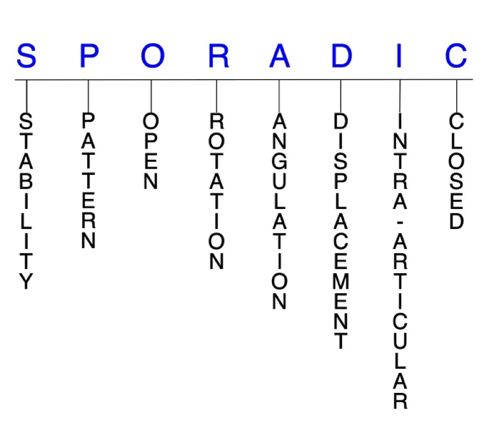
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.6-8
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable pisiform fractures have significant deformity with comminution, displacement and/or angulation.
- Most pisiform fractures are stable and can therefore be treated with immobilization alone.9
P - Pattern
- Pisiform proximal pole
- Pisiform distal pole
- Pisiform body: sagittal, parasagittal, coronal, transverse, and/or comminuted1,10
- Pisiform fractures are most commonly caused by either direct trauma to the hypothenar eminence—which is frequently seen in sporting activities—or tendon avulsion. Avulsion fractures occur when the flexor carpi ulnaris (FCU) tendon resists forcible hyperextension of the wrist, such as in a falls on an outstretched hand (FOOSH) injury or when straining to lift a heavy object, which can result in an osteochondral or avulsion fracture to the distal portion of the pisiform. A third mechanism postulated is repetitive trauma causing vascular disruption(AVN), microfractures, and eventually a complete fracture line.11,12 A fall FOOSH injury usually produces a transverse pisiform fracture by a combination of both direct and indirect mechanisms: the pisiform becomes fixed at the pisotriquetral joint when the outstretched hand strikes the ground, and forceful FCU contraction causes a transversely oriented avulsion fracture.1,11
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the pisiform require antibiotics with surgical irrigation and wound debridement.6,13,14
- Open pisiform fractures are exceedingly rare, with the first case in the literature being documented in 2013.3
- Open fractures of the pisiform may require surgical exploration to determine if articular surfaces are involved. After irrigation and debridement, these wounds are some times left open and further treatment is typically delayed until the wound shows no sign of infection.15,16
R - Rotation
- Pisiform fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- The pisiform can rotate up to 180° when it is dislocated but rotational deformity is rare.17
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- The small size of the pisiform makes assessing angulation between pisiform fracture fragments difficult.
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- Most pisiform fractures are nondisplaced, but they frequently demonstrate intra-articular extension.18
- The FCU is the wrist’s most powerful muscle, and the pisiform is a sesamoid bone that mechanically enhances its actions. Therefore, the pull of this muscle combined with forced wrist hyperextension associated with a FOOSH cause a significant traction to displace the pisiform proximally usually. In the presence of ulnar deviation associated with hyperextension of the wrist, the pisiform displaces medially.19
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Pisiform fractures can have fragment involvement with the triquetrum at the pisotriquetral joint.
- Although pisiform fractures are usually nondisplaced, most cases present with intra-articular extension.18
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly. Intra-articular fractures of the pisiform have a particular tendency to develop cartilage degeneration and osteoarthritis, which is why some argue for early mobilization without casting in these cases.20
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.6-8
Pisiform fractures: named fractures, fractures with eponyms and other special fractures
Pisiform dislocation and fracture-dislocation
- Pisiform dislocations and fracture-dislocations are very rarely reported, but it’s been suggested that many cases are missed and that their actual incidence may be higher.5,21,22
- Two mechanisms of injury have been described: a direct mechanism by which trauma is applied to the pisiform, and an indirect strong traction on the FCU tendon. Most pisiform dislocations occur through the latter injury mechanism, while the former is less common and often results in a pisiform fracture instead.21
- In the more common injury pattern, dislocation occurs with hyperextension traction of the FCU, which can tear the pisohamate and/or pisometacarpal ligaments. This can result from a FOOSH injury that causes significant traction to displace the pisiform proximally. If the pisohamate and pisometacarpal ligaments are damaged, the function of the FCU becomes impaired, with the pisiform retracting proximally.19
- Pisiform dislocation can occur in isolation or in conjunction with hamate dislocation, distal radius or ulna fractures, and/or other fractures/dislocations.2,5 In most cases, the pisiform dislocates distally and ventrally. There is no clear explanation why this occurs, but it may result from exaggerated physiological translation of the pisiform distally that normally occurs during wrist extension when it hyperextends. It could also result from the FCU tendon failing from being overstretched, or from injuries of ligaments that stabilize the pisotriquetral joint.5,21
- Common signs and symptoms include ulnar-sided hand pain aggravated by wrist flexion and adduction, swelling, tenderness, loss of hypothenar contour, exaggerated pisiform mobility, and ulnar nerve compression.2,5,21
Imaging
- Standard radiographic views of the wrist may be difficult to interpret and pisiform injuries may be missed or masked by associated wrist injuries. Oblique views usually require a comparison image of the contralateral wrist. In addition to standard radiographs of the wrist, a 30° or 45° oblique supinated view (ball cacher's view) is often needed to visualize the pisotriquetral joint.19,21
- CT scan is useful for suspected cases and can effectively demonstrate the integrity of the pisiform and identify any associated bony injuries.19,21
- MRI is also helpful for highlighting any ligamentous or ulnar nerve injuries present.19
Treatment
- Due to the rarity of pisiform dislocations, an optimal management strategy has not yet been identified.19
- Most experts recommend a conservative approach for acute dislocations initially, especially if ulnar nerve neurapraxia is present. This consists of immediate closed reduction using wrist flexion and forearm pronation, followed by immobilization with a splint or cast maintaining the reduced position for ~3 weeks.5,19
- In cases of recurrent dislocation, debilitating chronic pain, or when closed reduction is unsuccessful, surgery is typically needed and may consist of open reduction and internal fixation (ORIF) or pisiform resection or excision.5,19 Removal of the pisiform does not interfere with the normal functioning of the wrist.5
- When a pisiform dislocation is associated with a distal radius or ulnar fracture, treatment should address both injuries concomitantly.2
- If the FCU tendon, pisohamate or pisometacarpal ligaments are also damaged, they should be surgically repaired and probably best approached with repair of the FCU tendon possibly with a graft..19,21
Complications
- Infection
- Recurrent instability
- Osteoarthritis
- Synovitis
Outcomes
- Outcomes after closed or open reduction and immobilization are mixed, while pisiform resection has been found to offer a more predictable outcome. In cases of delayed diagnosis, resection is also preferred over reduction and is more likely to result in symptomatic relief.19 One reason open reduction leads to poor outcomes may be because it requires dissection, which can lead to more destabilization of the pisiform and damage to its blood supply.21
- Another study pointed out that good outcomes have been obtained without any treatment or splinting.21
Related Anatomy
- The pisiform is a small, pea-shaped sesamoid bone located in the most ulnar position of the proximal carpal row, on the volar aspect of the wrist. It consists of a distal pole, a proximal pole, and a body, and it articulates only with the triquetrum—which contributes no stability—on its slightly concave dorsal surface. Its volar surface is round and rough, and serves as an important point of attachment for the flexor retinaculum, the FCU tendon, and the origin of abductor digiti minimi. The pisiform also forms the ulnar wall of Guyon's canal, which is why ulnar nerve symptoms are common in pisiform injuries.5,11,12
- Ligamentous attachments of the pisiform include the flexor retinaculum, extensor retinaculum, and the pisohamate, pisometacarpal, and pisotriquetral ligaments, which maintain the position of the pisiform upon normal ROM of the wrist.The pisohamate and pisometacarpal ligaments, together with the ulnar part of the pisotriquetral ligament, are the primary stabilizers of the pisiform. There is also a superficial fibrous band that extends from the pisiform to the hook of hamate.1,2,11,12
- The pisiform is the only carpal bone that receives direct tendinous insertion, and the tendons associated with it include the FCUand the abductor digiti minimi. The pisiform is not completely embedded in the FCU, but it attaches to the tendon’s anterior surface, and it also forms an origin of the abductor digiti minimi. The FCU tendon continues distally to the pisohamate and pisometacarpal ligaments, which insert upon the hook of hamate and the bases of the ring and little metacarpals, respectively.2,5,12
- Carpal tunnel release can cause post-operative painful pisiform subluxation.
Incidence and Related injuries/conditions
- Fractures of the carpal bones have been found to account for 8-18% of all hand fractures23,24and ~6% of fractures overall.25
- Fractures of the proximal carpals are more common than the distal carpals, and the most commonly fractured carpal bone is the scaphoid, which represents 58-89% of all carpal fractures.23,24,26,27
- Fractures of the other 7 carpals are very rare and only account for ~1.1% of all fractures. The triquetrum ranks highest of these bones, while fractures of the remaining carpals are even less common and vary in incidence.28-30
- The incidence of pisiform fractures has been estimated at between 0.2-2% of all carpal fractures.11,24,27,31
- About 50% of pisiform fractures occur in isolation, while the other 50% are associated with other wrist injuries, such as a perilunate dislocation, distal radius fracture, or additional carpal fracture.1,11
Work-up Options
- Routine X-rays
- Pisiform fractures are difficult to recognize on routine radiographic views because of the fracture’s orientation, improper wrist positioning, superimposition of adjacent bones, or an inadequate number of projections. Nonetheless, it is advisable to use these films as the first step in evaluating possible pisiform fracture because they are readily available and inexpensive.
- A posteroanterior (PA) view will demonstrate transverse and sagittal fractures, while a lateral projection may show coronal fractures; however the pisiform may be obscured by overlapping other bones on both the lateral and standard oblique views.11
- Special X-ray views
- A 30° or 45° supinated oblique view in slight extension is helpful for demonstrating fractures in the coronal plane and also shows the pisotriquetral joint.10,11
- A carpal tunnel view is also beneficial for showing coronal fractures, but this view can be difficult to obtain in the acute setting, as dorsiflexion is limited by pain.10-12
- A clenched fist PA view with the wrist held in ulnar deviation may also assist the diagnosis.2
- CT scan
- Typically recommended if suspicion of fracture is high, other exams are negative, and the patient remains symptomatic, although some authors recommend systematic use of CT scan for all wrist injuries.3,11
- CT scans can provide useful additional information about fracture morphology and displacement, especially if they are not in the scan plane.2,11
- MRI
- Useful for confirming a pisiform fracture diagnosis, especially if radiographs were negative and suspicion remains. May show bone marrow edema within the pisiform, which can indicate a fracture and associated soft tissue injuries.4
- Bone scan
